Polyarteritis Nodosa
- Fysiobasen

- Dec 28, 2025
- 3 min read
Polyarteritis nodosa (PAN) is a systemic, inflammatory necrotizing vasculitis that primarily affects small- and medium-sized arteries¹. The inflammation involves the entire vessel wall, with a predilection for arterial branch points, and leads to fibrinoid necrosis and aneurysm formation¹. As the process evolves, thrombi can develop within inflamed segments, reducing perfusion to organs and tissues²—resulting in ischemia, infarction, and potentially life-threatening organ failure². PAN may involve the liver, kidneys, heart, gastrointestinal tract, testes, and skeletal muscle³. Without prompt, effective treatment, mortality is high, most commonly due to progressive renal failure or severe gastrointestinal complications³.

Etiology
The cause of PAN remains unknown, but the disease is presumed to reflect an autoimmune process triggered by factors such as drug reactions, viral infections, and immune mechanisms⁴. Clinically, drugs like iodides and penicillin have been associated with disease onset in predisposed individuals⁴. There is a strong link between PAN and active hepatitis B infection—20–30% of cases are HBsAg-positive⁵. Circulating HBV antigen–antibody immune complexes are believed to deposit in arterial walls and trigger the characteristic vasculitis⁵.
Epidemiology
PAN is uncommon, with an estimated incidence of ~2–9 per million per year⁶. It most often affects adults ages 50–70 and is roughly twice as common in men as in women⁶. Although HBV-associated PAN has declined in many countries following vaccine programs, clinicians must remain vigilant in regions with high HBV prevalence⁶.
Clinical Presentation
Systemic symptoms are often early and nonspecific⁷:
Fever, malaise, weight loss, night sweats
Over time, organ-specific features emerge, reflecting arterial ischemia/infarction⁷.
Common manifestations:
Skin: Palpable purpura, livedo reticularis, subcutaneous nodules, ulcerations—from cutaneous arterial vasculitis and highly suggestive diagnostically⁸.
Musculoskeletal: Myalgia, arthralgia, and diffuse muscle pain due to ischemia and inflammation⁸.
Peripheral nervous system: Mononeuritis multiplex—asymmetric weakness, numbness, paresthesia; wrist/foot drop is classic⁸.
Kidney: Hypertension, proteinuria, and renal insufficiency⁹.
Gastrointestinal: Abdominal pain, nausea, vomiting, bloody diarrhea—often from bowel ischemia/infarction⁹.
Cardiac: Angina and myocardial infarction if coronary arteries are involved⁹.
Hepatic: Hepatic injury; in severe cases, liver failure⁹.
Pharmacologic Treatment
Glucocorticoids are the cornerstone, rapidly suppressing inflammation and slowing progression¹⁰.
Prednisone/prednisolone is typically started at high dose, then tapered per clinical response¹⁰.
For severe disease or steroid-refractory cases, add cyclophosphamide as a stronger immunosuppressant¹⁰.
HBV-associated PAN requires a sequenced approach¹⁰:
Short course glucocorticoids (~2 weeks) to control vasculitis;
Then plasmapheresis plus antiviral therapy to lower viral load and immune activation.
Diagnosis
There is no single diagnostic test; diagnosis rests on integrating clinical, laboratory, imaging, and histopathology¹¹.
Labs: Systemic inflammation with elevated ESR/CRP, anemia; assess renal and hepatic function¹¹.
Angiography: May reveal microaneurysms in small/medium arteries—classically renal and mesenteric beds¹¹.
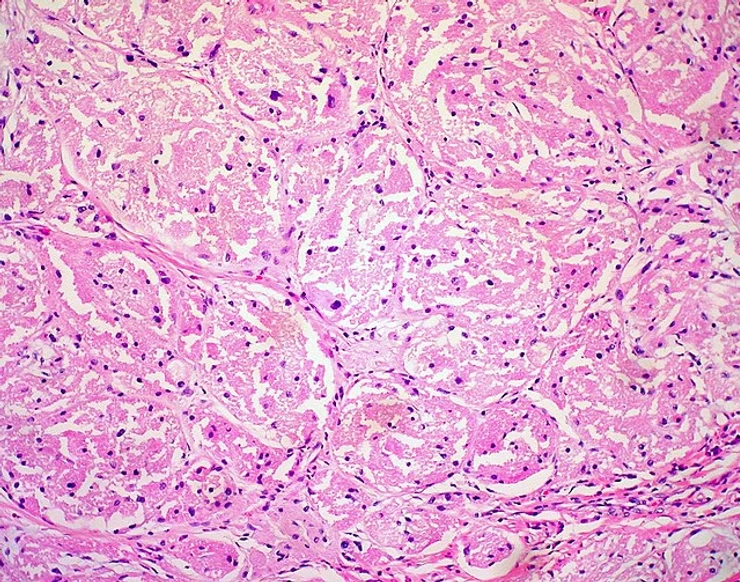
Biopsy (skin, muscle, nerve): Necrotizing arteritis of the vessel wall is diagnostic¹¹.
Surgical Treatment
Surgery may be required for acute GI complications—appendicitis, cholecystitis, pancreatitis, bowel perforation, or hemorrhage¹². Outcomes are generally poor in PAN emergencies, except appendicitis and cholecystitis, which tend to have relatively favorable results¹².
Emerging / Second-Line Therapies
For refractory PAN (especially non-HBV)¹³:
IVIG can be beneficial.
Anti–TNF-α therapy has been used in resistant cases.
Rituximab (B-cell–directed) shows promise in select patients.
Interferon-α has been proposed for mild HBV-associated PAN¹³.
Physiotherapeutic Management
While medical therapy is primary, physiotherapy is valuable once patients are medically stable¹⁴:
Goals: restore function, strength, and mobility; facilitate ADLs and safe return to activity¹⁴.
Principles: highly individualized programming given multisystem involvement; target functional limitations, aerobic capacity, strength, and energy conservation¹⁴.
Teamwork: close coordination with the medical team to monitor disease activity and adapt interventions¹⁴.
Differential Diagnosis
Consider—and distinguish from—other vasculitides and systemic diseases¹⁵:
Microscopic polyangiitis (MPA)
Rheumatoid vasculitis
Systemic lupus erythematosus (SLE)
Eosinophilic granulomatosis with polyangiitis (Churg–Strauss)
Careful clinical assessment, targeted labs, and imaging/biopsy are essential to separate these mimics from PAN¹⁵.
References
Radiopedia Polyarteritis nodosa :https://radiopaedia.org/articles/polyarteritis-nodosa-1
Merck Manual: polyarteritis nodosa. http://www.merckmanuals.com/home/sec05/ch069/ch069b.html
Cedars-Sinai: polyarteritis nodosa. http://www.cedars-sinai.edu/Patients/Health-Conditions/Polyarteritis-Nodosa.aspx
Goodman CC, Fuller KS. Pathology: Implications for the Physical Therapist. 3rd edition. St. Louis, Missouri: Saunders Elsevier, 2009.
Gjennomgått -Trukket
MedlinePlus Medical Encyclopedia: polyarteritis nodosa. http://www.nlm.nih.gov/medlineplus/ency/article/001438.htm
PubMed Health: polyarteritis nodosa. http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0002410
Lightfoot RW Jr, Michel BA, Bloch DA, Hunder GG, Zvaifler NJ, McShane DJ, et al. The American College of Rheumatology 1990 criteria for the classification of polyarteritis nodosa. Arthritis Rheum 1990;33:1088-93.
Johns Hopkins Vasculitis Center: polyarteritis nodosa. http://www.hopkinsvasculitis.org/types-vasculitis/polyarteritis-nodosa
Guillevin, L. Treatment of classic polyarteritis nodosa in 1999. Nephrol Dial Transplant.1999;14:2077-2079.
BMJ Evidence Centre: emerging treatments for polyarteritis nodosa. http://bestpractice.bmj.com/best-practice/monograph/351/treatment/emerging.html